Extravasation in Nuclear Medicine
Most nuclear medicine procedures involve an injection or an infusion of a radiopharmaceutical. The amount of administered radioactivity is critical to the quality of the procedure.
An infiltration (paravenous injection) is the inadvertent administration of a pharmaceutical into the tissue instead of the vein, as intended. Although an extravasation is typically defined as an infiltration of a vesicant, an infiltration of a radiopharmaceutical can be considered an extravasation due to the effects of ionizing radiation on patient tissue.
In many nuclear medicine procedures, precise dose information is necessary to accurately generate quantitative results. Standard practice is to measure the empty syringe in the well counter. Any residual radioactivity is subtracted from the original assayed value to establish an accurate net administered dose.
Extravasations and Quality
For many diagnostic imaging procedures, bolus injections (a volume of fluid injected rapidly) are a standard practice to deliver the radiopharmaceutical into the patient’s circulation. This ensures sufficient image contrast at time of imaging. Delivering a bolus also helps ensure consistency in the length of the uptake period, when comparing one image to another image.
For therapeutic delivery procedures, an extravasation prevents the complete delivery of the prescribed dose.
Extravasations and Quantification
Extravasations cause quantification errors that can affect image interpretation and patient management. They impact both the dose available to the patient during uptake and the effective length of the uptake period–both key quality indicators. Radiopharmaceutical remaining near the administration site means that some portion of the radioactivity is not circulating as required for the prescribed uptake period.
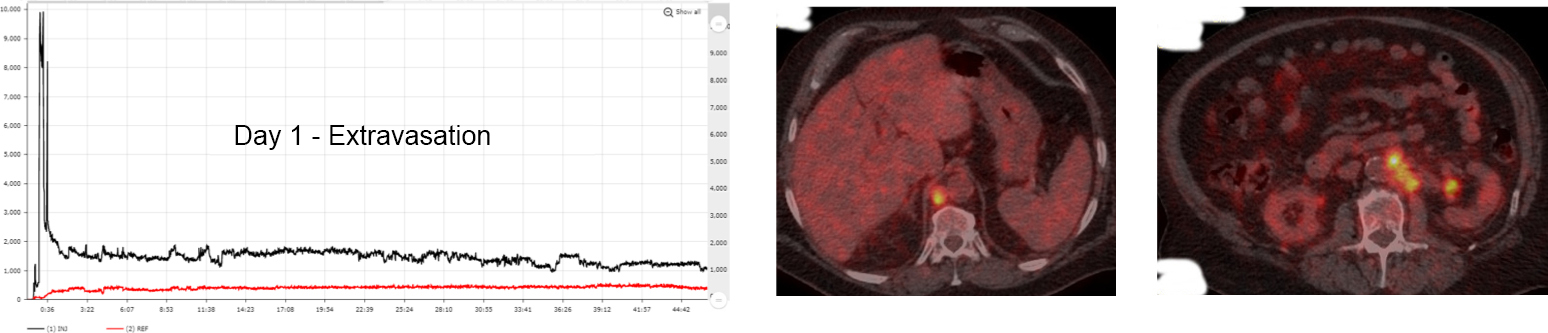
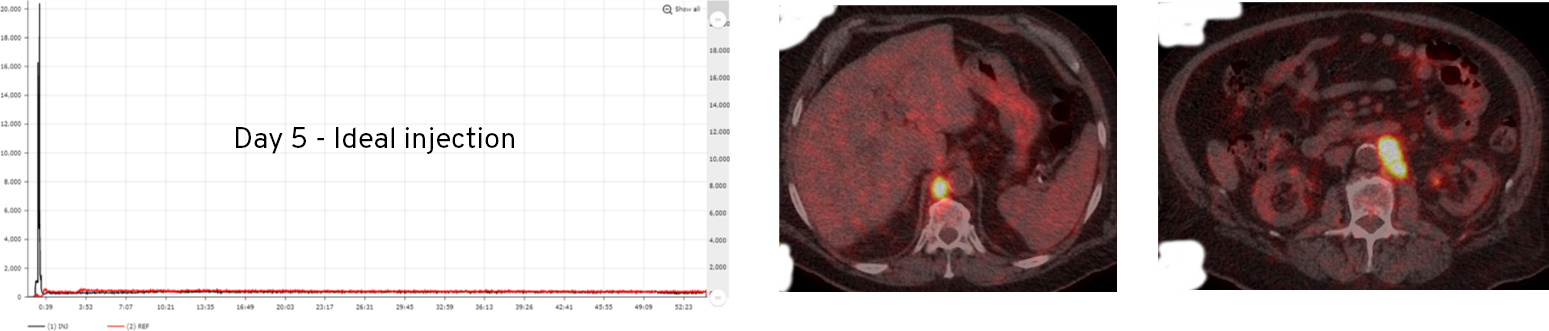
In the case below from a test-retest clinical study, the administration site was out of the imaging FOV, but the patient experienced a significant extravasation that was identified by Lara and confirmed when the patient returned five days later for re-scan. The principal investigator determined that the quantification of these metastatic lesions was understated between 30-70% due to the extravasation (patient and protocol preparations were consistent between imaging studies to minimize variation between procedures).
Extravasations can irradiate patients’ tissue with high doses
An extravasation unintentionally irradiates the patient’s tissue with more radiation than prescribed. As the radiotracer decays within the arm tissue, it emits energy that absorbed locally. Dose is calculated as absorbed energy divided by mass. The absorbed dose to the infiltrated tissue is much higher than it would have been without an extravasation. High doses can lead to adverse tissue effects and increased risk of cancer.
Extravasations are surprisingly common
While there is not much public information available regarding radiopharmaceutical extravasation rates, 31 centers have published their extravasation rates (average of 17.2%). A recent quality improvement project of radiopharmaceutical administrations in seven centers involving 2531 patients supports the previously published extravasation rates. With 18.5 million nuclear medicine procedures in the United States each year involving ~30M radiopharmaceutical administrations, it is likely 4.5M patients are extravasated every year. Of these, ~500K+ patients may be harmed by significant extravasations* each year.
*Company estimates based on 28,000+ monitored injections
Current tools to capture extravasations are inadequate
In many nuclear medicine studies, the administration site is outside the imaging field of view, so physicians and patients have no idea that an extravasation happened. A recent study* indicates that approximately one third of all extravasations may not be visible to clinicians interpreting the images based on the imaging field of view (FOV). In our experience, the administration site can be out of the field of view even more frequently. In over 28,000 procedures monitored with the Lara System, the administration site is likely out of the FOV in ~50% of the images.
Even when extravasations are in the FOV, the static image cannot provide true insight into the extent of the extravasation over time.
Without insight into the uptake process, physicians and patients cannot be sure if the administration was ideal. As a result, patient management decisions may be compromised, and patient tissue may be irradiated with high levels of unintentional radiation.
The Lara System provides a solution that takes nuclear medicine to the next level of quality.
