On average, every 56 seconds in the United States, a nuclear medicine patient is significantly extravasated.
It could be you, a family member, or a friend.
We need your help to fix this patient safety issue.
- Learn more below
- Contact the NRC and your members of Congress
- Share this page with others

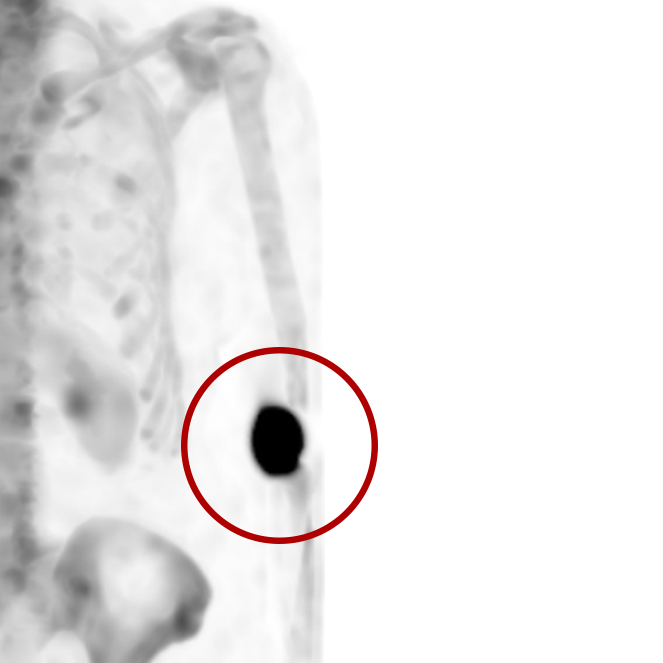
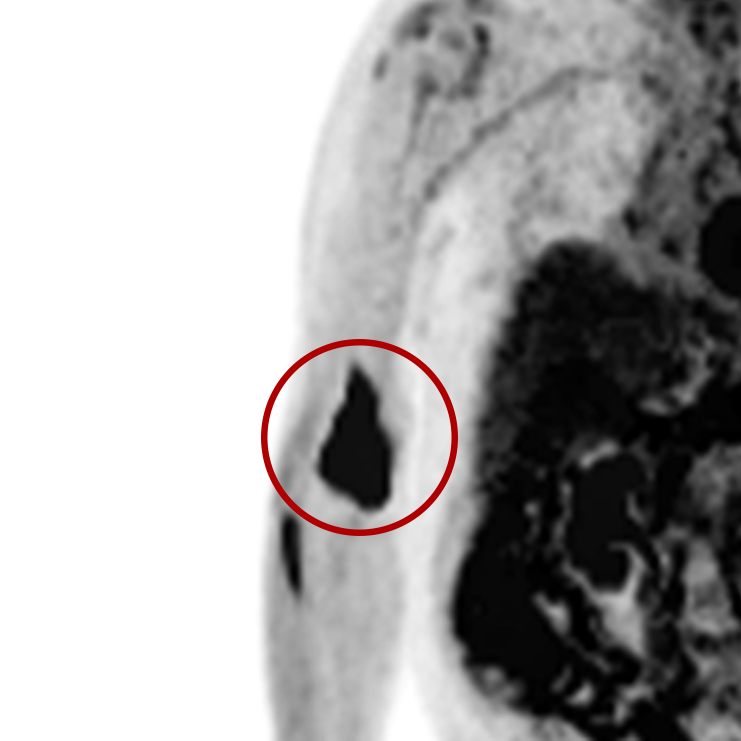
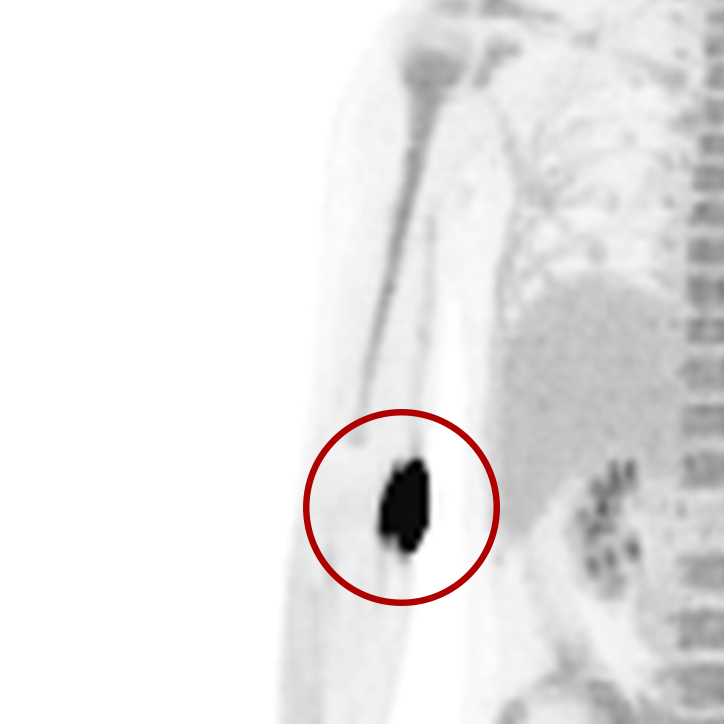
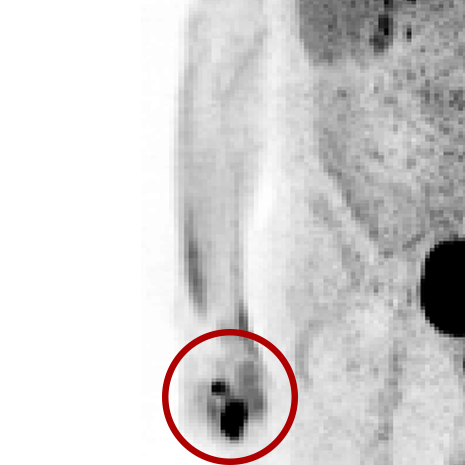
Extravasations are circled in red
An extravasation is the misadministration of a radioactive drug
For nuclear medicine procedures, a technologist injects/infuses a radioactive drug (radiopharmaceutical) into a patient’s venous system. An extravasation, also known as an infiltration, occurs when some or all of the radiopharmaceutical is inadvertently delivered into the patient’s tissue rather than their vein. Extravasations occur frequently at many nuclear medicine centers and negatively affect patient safety and care.
1,500+ patients experience significant extravasations every day
Annually
*Company estimates based on 20,000+ monitored injections
Extravasations can harm patients
(watch video)
Extravasations can compromise patient care
- Diagnostic extravasation: results in misinterpretation of medical images
- Therapy extravasation: prevents the delivery of the prescribed radioactive treatment
Extravasations can unintentionally irradiate patient tissue with high doses
- Leads to adverse tissue reaction months to years later
- Increases risk of cancer at the injection site
Food and Drug Administration and
Nuclear Regulatory Commission regulate nuclear medicine
FDA
Approves radiopharmaceuticals and nuclear medicine equipment
NRC
Assures the proper medical use of
radiopharmaceuticals and protects patients from unnecessary radiation
The NRC’s 1980 policy fails to protect the safety of patients
May 1980 NRC actions
- established misadministration reporting regulations
- exempted extravasation from reporting
- exemption is an internal policy (not a regulation)
- policy based on belief that extravasations occur frequently and are “virtually impossible to avoid.”
Extravasations are NOT virtually impossible to avoid
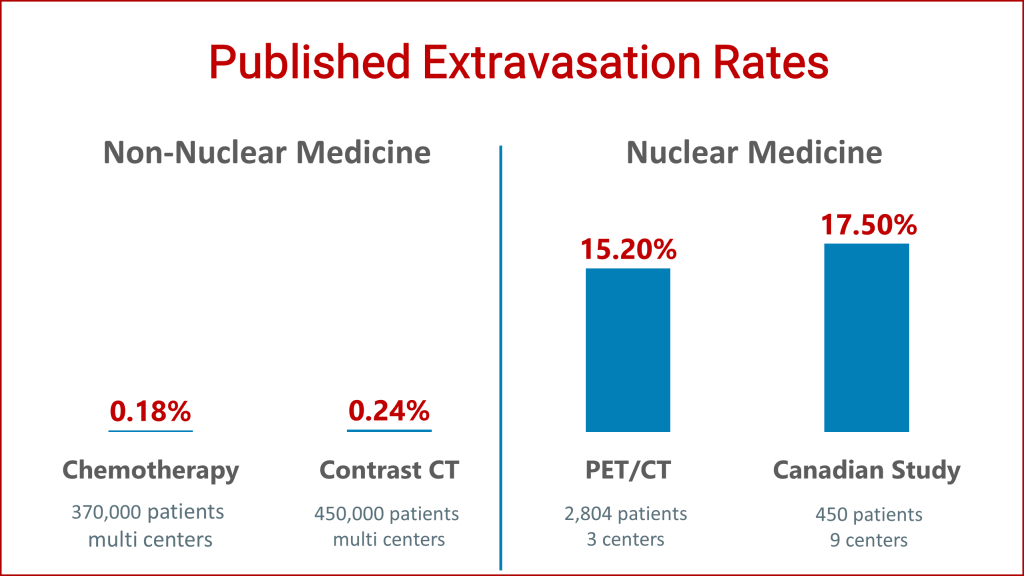
Chemotherapy and contrast CT administrations are similar to those in nuclear medicine. In the 1990s and 2000s, chemotherapy and contrast CT extravasation rates were significantly improved because of quality improvement projects.
In 2019, the world’s largest nuclear medicine injection quality improvement project was published. It demonstrated that nuclear medicine centers can also significantly improve their extravasation rates. The NRC is now aware of all of these results.
The Association for Vascular Access, whose mission is to protect and save lives by establishing best practices and promoting the vascular access specialty, agrees that extravasations are NOT virtually impossible to avoid and provided a comment to the NRC. Here is what these experts said:
The NRC exemption policy results in the following paradox:
a radiation spill ON a patient is reportable, but an extravasation INTO the patient is not
A proper radiopharmaceutical injection irradiates patient’s tissue with a harmless dose of ~1 millisievert (mSv).
The NRC has established 500 mSv as the reporting limit for misadministrations.
An accidental radiopharmaceutical spill ON the patient which exceeds 500 mSv exposure to patient tissue is reportable. However, an extravasation INTO the patient is not reportable….even when the tissue dose far exceeds 500 mSv.
Extravasations can grossly exceed NRC limits
Therapy extravasations are well-known to exceed the NRC reporting limit and have resulted in patient harm.
Diagnostic extravasations can also exceed 500 mSv – Lucerno has shared 36 examples with the NRC. Few patients, if any, are informed when this happens to them.
MDP Bone Scan Patient

Dose Equivalent – 31,300 mSv
Lucerno officially petitioned the NRC to change their regulation
After 18 months of effort to address the 1980 policy, Lucerno officially petitioned the NRC to eliminate the extravasation reporting exemption. While the NRC official public comment period is closed, it is not too late to help close this regulatory loophole.
The public comment period revealed a lack of understanding regarding several aspects of extravasations
The process of tissue injury due to ionizing radiation may take weeks to years to appear depending on the tissue and the absorbed radiation dose. For some extravasations, it is likely that underlying tissue will absorb significantly more dose than the skin.
Also, there is conclusive evidence that extravasations are due to tools, training, and technique used during the administration of radiopharmaceuticals. They are not the fault of the patient.
Over the past 40 years, nuclear medicine providers have failed to reduce the incidence of extravasation through internal means and it is unlikely that the community will fix this problem voluntarily. Additionally, accreditation organizations (ACR, IAC, and the Joint Commission) have no requirements related to extravasations in nuclear medicine.
While the four nuclear medicine societies confirm that extravasations can negatively affect image quality and quantification, many nuclear medicine professionals still don’t think image quality and quantification are issues that harm patients. The literature is clear on this point—extravasations can result in inappropriate care.
Many comments suggest that patients should not be told when they are significantly extravasated. This belief is inconsistent with the practice of modern medicine; patients want to know about information that can affect their care and need to be informed.
Here’s what others have submitted to the NRC or published on the need for changing the regulation
- Here are comments from regulators: Organization of Agreement States and Arkansas Department of Health Radiation Control Section
- Patients, families, and advocates also want the loophole closed: Comment 367, Comment 358, Comment 419, Comment 435
- Here is what the CEO of the Leapfrog Group, a leading healthcare transparency organization, thinks about the petition: Comment 030
- Patient safety is a bi-partisan issue. Several members of Congress, Senator Thom Tillis, and Congressmen David Price, George Holding, G.K. Butterfield, Denver Riggleman, Ben Cline, and Congresswoman Lucy McBath supported the petition by submitting public comments: Comment 019, Comment 373
- Several members of nuclear medicine and radiology community also believe significant extravasations should be reported: Comment 002, Comment 021, Comment 202, Comment 414, Comment 368, Comment 028
- Here are some other powerful comments: Comment 341, Comment 325
- And the co-inventor of the PET/CT scanner, Dr. David Townsend, has written two separate articles on the need to change the regulation: STAT and ARRS InPractice
It is not too late to help close this loophole
Points to consider when submitting comments
Submit a comment directly to the NRC or contact your legislator
To submit a comment to the NRC, please click here.
- In the “Public Affairs Location” section, select Washington, DC.
- In “Subject” section, include “PRM-35-22”.
We also recommend notifying your legislator about this patient safety issue.
- Find your Senator or Representative and send them an email.